Blog

A year goes by, time ticks on, we grow, we further our missions in life. This year was the year of music growth for me as a human. What does it mean to truly care for your fellow human and to use music as a catalyst to care for them? I garnered a lot of ways to do this in a year. What is the main thing I learned? Listening. What truly is the art of listening? I focused heavily on my 10 domains of care. The one I honed in on the most was environmental sound. The environment impacts us all, it’s our scope. The little things count, a movement. It can be a rhapsody, it can be fingernails on a chalk board. I focused on rhapsody and said hello to chalk board screeches. How could I make sounds more pleasant? I adjusted volumes to devices, tones, pitches. I created musical soundscapes that fit the unique quality of the human condition within our realm. I listened with quenches or smiles, I aimed for relieved looks, looks that said, “this sounds right.” I chose sounds that spoke to the tribe. When I worked one on one, I spoke to the spirit of the one. I’m listening to Bob Seger writing this and his song, “Against the Wind.” That’s what I did this year; I ran against the wind. I tackled an inevitable, sounds. Sound should speak to us all, not turn off our volume. I also learned how to help, not only myself cope with unpleasant sounds, but my folks I care for too. The answer? It lies in the acceptance. Call it out- admit it’s way of making you feel. Feel, hear, react, adapt. So, this year as I ran against the wind? The wind began to become a song instead of a gush. It now is more of an orchestra at our facility. Each little hiss, buzz, ring, ding, ting or veritable element of sound is something part of an accepted orchestra. Each or us tuned into our humanness here, in our domain. I also launched our own record label. It’s called Gentog Records, named after our mission. Generations together. We launched our first single to major distributors, it is called, “New Beginnings.” It is music written and inspired by humans dealing with neurodegenerative disorders with me as their Sherpa. It represents a big no to what we call “disease”. It shows that humanity and dignity exist, despite it all; the human spirit is the definition. The label is two-fold. 1) To offer ownership and authorship as creators over their sounds and over their feelings and stories. 2) Generate income for the non-profit we have Gentog Community Services. It’s been a year, one of triumph and failure. Still here we are, perhaps still running against the wind. But, bring on the wind! Embrace its orchestral movement. I know one thing for sure, I’m more in love with sound and humanity. And that, that sounds lovely.

As a psychologist and a researcher, I spend my days exploring the incredible benefits arts engagement can bring to the health and well-being of individuals across the lifespan. A particular focus of my work is on music, be it group singing in choirs, intergenerational music therapy that connects young children from the community with residents of long-term care homes, virtual opportunities for families to sing together from a distance, or high-quality concerts provided by professional musicians. Given my background, you’re probably wondering how I ended up leading a holiday sing-along with Toronto Mayor Olivia Chow in November… My current role is the perfect match for my longstanding interest in the arts. My love of music began at an early age. As I was the only niece living close by, I was my aunt’s regular “plus 1” for all sorts of musical performances coming through Montreal’s Place des Arts and Bell Centre. Growing up singing in choirs at church and in high school led to performances with the Hart House Singers when I moved to Toronto for graduate school. Over the last few years, my singing has been more commonly directed to an audience of two small children (and a cat), and I’ve harnessed my love of group singing into my research: I am currently involved with the SingWell project, an initiative out of Toronto Metropolitan University that examines physiological and quality of life benefits of group singing for a variety of populations, including individuals living with hearing loss, Parkinson’s disease, and dementia. So imagine my surprise and delight when I recently had a powerful reminder of the personal joy of group singing. One chilly day in November, I had the opportunity to walk in my local Santa Claus parade with the Mayor of Toronto. As we neared the end of the parade route, there was a bend in the road where our group decided to set up and play some holiday tunes. Unfortunately, it seemed as though the sound system was out of order, and Mayor Chow turned to the group and asked “who likes to sing”? I sprang to respond, flung up my hand, and was immediately brought to the front of our crowd and found myself- unexpectedly and delightedly- leading an extremely enthusiastic and joyful choir on a street corner just blocks from my home! We sang for about 15 minutes, cycling through a repertoire of tried and true holiday favourites, sometimes stumbling over the words, sometimes getting an assist from people passing by! Folks who were completing their own parade journey, joined in, sang along, shouted encouragement, smiled and waving as they passed. While singing, my inner scientist couldn't help but wonder- were my cortisol levels decreasing? Maybe my oxytocin, the human bonding hormone, was shooting through the roof! This unique opportunity was the perfect representation of so much of the work I have been doing for many years. Seeing so many faces breaking into smile (and so many people breaking into song!) was a keen reminder of the power of music to connect us, and emphasized the important work that the room 217 team does every single day.
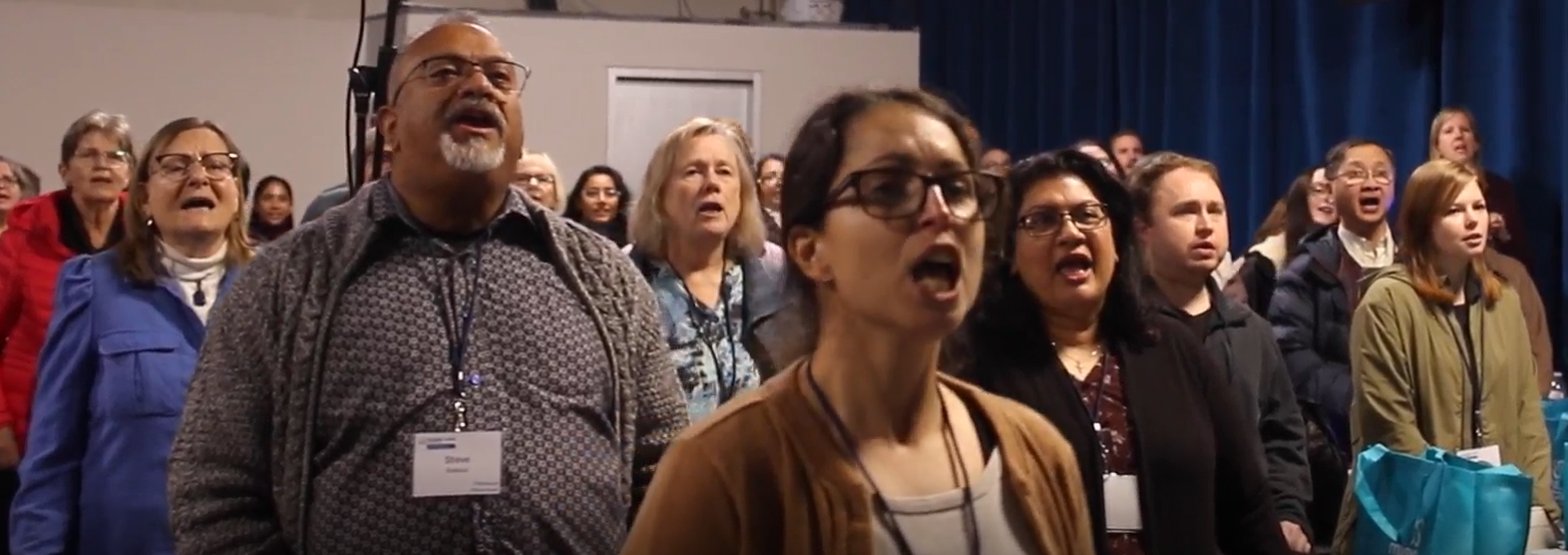
There are conferences that inform, inspire, and educate, and then there are conferences that change how we imagine what care can feel like. The Music Care Conference: The Power of a Song in Dementia Care, held at Metalworks Institute in Mississauga, was one of those rare experiences. Positioned as a national gathering that brings together people engaged in music in care across clinical, community, and educational settings, the purpose of the day became clear right from the beginning. This was not a passive event; it was an active space for co-creation and genuine connection. From the moment participants arrived, the atmosphere felt more like the start of something being built together. One of the most profound moments came during a workshop led by Bev Foster, where attendees from diverse backgrounds were to record a song together. There was no expectation of musical training or polished performance. The invitation was simply to contribute a voice and be part of the process. The piece we created was titled ‘Without a Song,’ written by Canadian singer songwriter Murray McLauchlan, and in that moment it became a shared expression of care and connection. What began as a room full of strangers gradually shifted into a connected musical space. People leaned in, listened closely, and began to sing together with growing confidence. It felt less like watching music happen and more like becoming part of something shared. In that moment, the workshop no longer felt like a breakout session. It became a living example of care expressed through music. This experience carried particular meaning in the context of dementia care. When language shifts or memory becomes harder to access, music offers a different pathway to connection, one grounded in presence. Creating music together invites participation rather than observation and can restore a sense of agency for people whose autonomy is often limited by care environments. It also strengthens relationships between caregivers and the people they support. Music does not sit on the edges of care as an added activity. It can function as care itself. The conference also highlighted that the role of music in dementia care is part of a broader shift in how the sector is evolving. With growing momentum around Bill 121, the Improving Dementia Care in Ontario Act, and increased attention from the Ministry of Long-Term Care, music is beginning to be recognized as a meaningful part of care. This commitment was reflected in a heartfelt address from Minister of Long-Term Care, Natalia Kusendova-Bashta, whose remarks affirmed the importance of dignity and compassion in dementia support. At one point she held her son at the podium and led the room in a playful rendition of ‘Baby Shark’, a moment that demonstrated how music creates connection across generations and circumstances. Policy can outline goals, but experiences like this help us imagine what care feels like when creativity and connection guide the approach. Throughout the day, research and lived practice came together through presentations from experts such as Dr. Lee Bartel, Dr. Alison Sekuler and Taylor Kurta, and through examples from organizations already integrating music-based programs in long-term care and community settings. Although the collaborative songwriting session stood out, it was one part of a day filled with meaningful experiences. The Raising Voices Dementia Choir demonstrated how music can help people living with dementia stay connected to their identity and to the people who support them. Later, the closing performance by Jill Barber brought a different dimension to the day, weaving artistry, memory, and personal storytelling into a musical experience that resonated deeply with the audience. The day also highlighted new models of community engagement such as the ‘Memories to Music’ songwriting project between the Alzheimer Society of Peel and students from Mentor College. Led by music teacher Ian Hoare and music therapist Ruth Watkiss, this initiative brings young people and persons living with dementia together to create original music, demonstrating how intergenerational collaboration can strengthen understanding and relationships across care settings. As I left the conference, I kept returning to the responsibility that comes with making music together in a care context. The song we created did not end when the session wrapped up; it became a reminder of what can happen when care is grounded in creativity and shared voice. If a group of people with no prior relationship can come together and create a shared musical experience in such a short time, then there is potential to bring this same approach into long-term care homes, community programs, hospitals, and family caregiving settings. These environments are already spaces of deep commitment and compassion, and with the right intention and support, music can help deepen relationships and strengthen the culture of care. The power of music in care is not found in adding it as a program feature; it comes from recognizing it as a way of relating to people with dignity and presence. When music becomes a shared experience, people living with dementia are included and understood rather than defined by their diagnosis. This work continues through collaborations with partners such as Acclaim Health, the Alzheimer Society of Peel, ArtsCare Mississauga, and Metalworks Institute, who help create environments where music supports meaningful connection. The music eventually came to an end, yet the song stayed with me as more than a moment from the day. It became a reminder of what can happen when care is grounded in creativity and shared voice. I left the conference with a clearer sense of how music can shape the way we support one another in real and meaningful ways. As we look ahead to the next Music Care Conference in Halifax in 2026, we carry this momentum forward, knowing that none of it happens ‘without a song’ to bring us together.

In the first two blogs of this series, we explored why music is such a powerful tool in dementia care—how it can connect with the “preserved self” and awaken memories and emotions that remain intact despite cognitive decline. Research consistently shows that music positively influences every dimension of human experience, from our physical responses to our emotional and social well-being. The question remains. How do we use music everyday in dementia care? Let’s consider some daily scenarios and match a musical strategy to use in care situations. These are not prescriptive, rather musical approaches that need to be used purposefully, being mindful of an individual’s response. As a carer, pay attention to the effect of the music. If you can see it is supporting an individual, continue. If not, stop and try something else. Here are nine musical strategies to be used for a particular purpose. The key to music care is that you are being intentional about what you’re doing and mindful of the effects. The goal is to support an individual’s health and wellbeing. Hum for Sleep For many people, humming is less intimidating than singing. Humming facilitates self-soothing which becomes by extension soothing for those around us. In this way humming invites presence, attuning us to the moment, concentrating on the experience of sound and vibration, and its effects on the breath and body. Gently humming a favourite song, or two or three pitches, perhaps with stroking a hand or cheekbone area may be calming and relaxing and help someone become drowsy. Play an Instrument When Someone Wanders Wandering and getting lost suggest the person living with dementia is bored or they may be looking for someone or something. One way to address this distraction is to change the soundscape by playing an instrument, such as a shaker or a hand drum. The sound may shift their focus towards the sound source drawing them into listening and perhaps engaging them in playing an instrument. You can also extend this connection by playing along to some recorded music, together. Play Calming Music at Mealtimes Proactively using music 30 minutes prior to any activity that’s being supported will boost cognition and trigger the brain in advance of the activity. In the context of mealtime, using music will help prepare an individual to recognize their food, swallow, and perhaps, increase intake. Use Singing Games to Improve Mood A way to immediately shift the mood of an individual or invite engagement with a group who may be anxious because they don’t know each other well is to play a fun and simple game using a well-known song, like My Bonnie. Sing the song a few times with the individual or group and then add an extra challenge like clapping hands on every word that begins with “B”. This kind of simple singing game can come with loads of laughs and fun. Use Designed Music for Sundowning The tempo and energy of music can potentially agitate a person living with dementia. It also has the potential to calm. Room 217 has a library of designed music. For example, the four MUSIC COLLECTIONS are ideal for calming. Paced at 60 beats per minute to sync up with resting heart rate, this music, which is mostly familiar Western music, tends to have a calming, comforting effect. The PATHWAYS Singing Program, 30 minute episodes of familiar songs led by a singing host, is purposefully designed for engagement. Individuals are invited to sing. This engaging program has resulted in less falls, and a deeper sense of belonging. You can find these tools at the MUSIC CARE Store , or on the MUSIC CARE CONNECT streaming app available on Google Play or the Apple Store . Dance for Exercise Research tells us that music and dance together are the most brain nourishing activity. Not only can dance be a stimulating and enjoyable way to move the body, it can also help to release tension and release energy. Dancing together is a bonding experience that can bring a sense of community to a group. Use One Song for Cuing and Recognition A favourite music care strategy is called ‘One Song.’ Choose one song, or a phrase/chorus of a song for a particular activity and use that song – whether you sing it, whistle it or hum it each time that activity is to occur. Ideally, the one song has particular meaning to the individual living with dementia. For example, Use a Personal Playlist for Personal Care This time of the day can be particularly challenging. Using someone’s favorite music can lighten these care tasks. Sing along, “celebrate good time times, come on!” when wanting to transition an individual or group from lunch or a nap to an activity or a program. Breathe Together for Deeper Connection Being aware of your own breath can make a significant impact on our caring relationships. Humans entrain, or sync up, with each other’s breathing. This mutuality has implications for how individuals experience their care. So be aware and present to your own breath. Is it deep or shallow? What is the pace? Where does it land in your body? Are you breathing from your nose or mouth or both? Then become aware of the other person’s breathing. Pay attention to how they are breathing. Then consciously change your breath to match their breath. You may use these strategies interchangeably. The more confident you can become with each strategy, the more they become part of your daily practice and valuable assets in your caregiving toolkit.

We know that as we age, our memory is one of the first things to shift. For someone living with dementia, this can be especially profound, short-term memory is often the first to fade, while the past can sometimes linger in unexpected and beautiful ways. I saw this firsthand with two women I loved deeply: my grandma, Hilda, who lived with vascular dementia, and my mother-in-law, Elma, who lived with Alzheimer’s disease. In both of their journeys, one thing consistently bridged the growing gap between their world and ours: music. Music wasn’t just background noise. It became the heartbeat of our visits. It was the thing that reached beyond confusion, beyond silence, and connected us to each other and to lifetimes of memories. Dr. Oliver Sacks, the renowned neurologist, said that music is the most powerful care modality for people living with dementia because it can find the preserved self. This couldn’t be more true. Music has a unique ability to nourish neural pathways and access multiple parts of the brain. This is one reason why music is powerful in dementia care, because music may not be completely lost. If one pathway is blocked, another might still be open. Every visit with Hilda and Elma had its soundtrack. We played the songs they loved, the ones that carried meaning from their lives. Those familiar melodies weren’t just entertainment, they were a bridge. A bridge to stories, to laughter, to their preserved selves. One of the most moving examples of music’s power comes from a widely shared video of Gladys Wilson and Dr. Naomi Feil , filmed by Memory Bridge. Gladys, who lives in a nursing home, did not know Naomi before their encounter. Yet through music, a remarkable connection unfolds. As Naomi sings an old spiritual song, something changes in Gladys. First, her hand starts tapping to the rhythm. Then comes an intentional gesture, she reaches for Naomi. Her eyes open. She begins to hum, then to sing, then to speak. This isn’t just a musical interaction; it’s a moment of awakening. The connection is both intrapersonal (Gladys reconnecting with herself) and interpersonal (a bond forming between her and Naomi). Through gentle touch, eye contact, and allowing the moment to unfold slowly, trust blooms. And, perhaps most powerfully, Gladys’ sense of rhythm becomes the guide. Naomi follows her lead. The songs chosen are the ones that matter to Gladys. In just five minutes, music brings Gladys back to herself. It doesn’t erase her dementia, but it reminds her, and those around her, of who she is. Music has this extraordinary way of helping us trace our personal narratives. For those living with dementia, these narratives can become hard to access through words alone. But a familiar melody can open doors that seemed locked. These musical moments aren’t just about singing songs, they are about connection. They are about love, identity, and belonging. With Hilda and Elma, these moments gave us something precious: a way to meet them where they were, not where memory used to be. Music may not cure dementia, but it can bring light into its shadows. It can awaken parts of a person that illness cannot fully erase. If you’re caring for someone living with dementia, consider exploring their musical past. Play their favorite songs. Sing together. Let the rhythm guide the moment. Because in those musical moments, something sacred happens: We don’t just remember the music, the music remembers us.

Music is more than just background noise — it’s the soundtrack to our lives. It connects us to memories, people, and emotions. It lifts us up, calms us down, and brings us back to moments we thought we’d forgotten. That’s why, when it comes to dementia care, music isn't just helpful — it can be transformative. Even as other parts of the brain struggle with language or short-term memory, music has this remarkable ability to break through. And research backs that up. Here are 10 reasons why music is such a powerful tool for supporting individuals living with dementia. 1. Music Sparks Memory - You’ve probably seen it before — someone who struggles to remember names or faces suddenly lights up when they hear an old favorite tune. That’s because music is stored across many areas of the brain, not just one. So even when dementia causes some areas to decline, others may still recognize melody, lyrics, rhythm, and harmony. That multi-area storage makes music a resilient memory trigger. 2. The Brain Can Rewire Itself (Yes, Really) - Thanks to neuroplasticity, the brain can adapt and form new connections — even around damaged areas. For some people with dementia, this means that new songs or even new skills can still be learned. That’s hope in action. 3. Music Unlocks Emotional Memories - Certain songs instantly take us back — to a wedding, a childhood home, a loved one. For people with dementia, these emotional ties can unlock memories thought to be lost. Why? Because emotions are powerful memory anchors, and music naturally brings emotions to the surface. 4. Music Offers a Way to Communicate - Even when words fail, music speaks. Take the example of Gladys Wilson and Dr. Naomi Feil’s touching moment (watch it here ). Through music, Gladys — who no longer used words — found a way to connect, respond, and express herself. Her rhythmic tapping became a language of its own. 5. Personalized Playlists Make a Big Difference - Familiar music — especially songs someone loved earlier in life — can be incredibly powerful. Research shows that preferred music can reduce agitation, soothe anxiety, and even help preserve a sense of identity. So yes, playlists really do matter. 6. The Carryover Effect is Real - One of the most remarkable things about music in dementia care is its lasting impact. After engaging with music, a person might show improved mood or awareness not just for minutes — but for hours, even weeks. While it’s not guaranteed every time, this “carryover effect” shows how deeply music can reach. 7. Music Meets Social & Emotional Needs - Singing together, drumming, or just sharing a favorite song can create connection and improve quality of life. Music addresses core psychosocial needs — like inclusion, comfort, and belonging — that are so important for people living with dementia. 8. Family & Caregivers Can Join In - You don’t need to be a music therapist to make a difference. Simple activities like singing with a loved one, humming during care routines, or playing familiar tunes while helping someone get dressed can turn routine tasks into meaningful moments. 9. Music Supports Every Stage of Dementia - From early stages to end-of-life care, music continues to offer value. In the early days, it can jog memory. In the middle stages, singing can help with focus and cognition. And in late stages, music provides comfort, connection, and even dignity. It’s never too early or too late to start. 10. Music Pairs Beautifully With Other Therapies - Music doesn’t have to stand alone. It works wonderfully with art, dance, cooking, and storytelling — enhancing experiences and deepening engagement. Whether it’s part of a craft session or simple dance movement, music makes everything more joyful and meaningful. If you’re caring for someone with dementia — as a family member, nurse, or caregiver — remember this: you already have one of the most powerful tools at your fingertips. A favorite song. A melody from the past. A gentle rhythm. Music doesn’t just bring back memories. It brings back connection, expression, and sometimes, even joy. So go ahead — press play.

And here we are together again, friends, for a third and closing reflection in this series of musical musings. You have graciously come alongside, and I am deeply grateful. Those who have explored sound and song with me in recent years know to expect that, before we turn our eyes to any musical scores, I will draw you into a small ritual of intentional breathing as we step into our shared time and space. As an advocate for music’s capacity to foster our wellness, I lean on the power of our breath to open a portal into that collective creativity. I hope that you all will also play along with me for just a moment, preparing yourself for reading the musical care vignette I am sharing with you here. As this week comes to a close , what piece of music is calling you to listen, to truly listen? Carve out a little more time to find it just now on your preferred platform and simply press ‘play ’. For me, first to mind is Samuel Barber’s Adagio for Strings, performed by the New York Philharmonic under the ever-intuitive baton of Leonard Bernstein in the 1960s. This recording honours the rests as much as the notes, with ample breathing room for an intentional practice like ours. Now, make yourself comfortable, either standing with both feet grounded on the floor beneath you or, if seated, on the chair’s edge such that you are aware of your posture. During a conducting workshop several years ago, the concepts of sinking with strength into our inhale and rising with lightness as we exhale resonated such that I have woven them into my care approach, to always invite others to find this breathing pattern in preparation for musical engagement. Close your eyes if you are able and just feel your whole self melt into this moment. Take your time … these written words below can await your return:) “Emotion in song. I want all of it.” When I heard this desire expressed by the narrating character of a current film in theatres “The History of Sound” I thought yes …yes, so do I, for what are songs but stories set to melody, evoking deep emotions? One of my community partners aims to offer lifestyle interventions of movement and creativity for those living with brain conditions and their care partners. It is my joy to facilitate a virtual singing collective for them as well as in person collaborations where sounding and singing flow into our pursuit of connection and wellness. It is through one of these workshops that an opportunity has arisen to offer music as care to an historian in his eighties recently diagnosed with Alzheimer’s. He is hoping that singing fervently like he did in the choir of his youth will soften the edges of the grief he has been carrying since his childhood. Emotional expression is at the very core of our time together. On the wings of song and tears, our shared experience is heartbreaking and healing all at once. It is one of life’s stunning beauties that music can be this gift to us, reaffirmed by a live performance that brought me to tears last evening by The Swell Season. I have been playing their most recent album on repeat all morning, each song resonating deeply. Seek this out for yourself, my friends. Let music wash over you, release you, ground you, and connect you to your loved ones. In so doing, you are crafting another meaningful chapter of your personal story.

Well hello again, friends. Buoyed up by hope that my words offered here a few weeks ago have had you considering your own unique moments of being touched by music as care, I will sharpen our shared lens and share another vignette of personal experience. I have been making music in church spaces since I was very young…it is a give and take that has woven into my life rhythms as a constant beat for almost fifty years. The gratitude piece that flows through this element of musical practice is that my family of faith granted me a formative foundation from which to understand music as a spiritual gift of care. So, to recently have a woman with whom I worship Sunday after Sunday express with eloquence what it means to her to receive my playing and singing, it moved me deeply and felt worth sharing here. She is a spiritual care practitioner and a visual artist. She sees and experiences the most profound of feelings on the daily. Bonding over coffee and platz , she graced me with a beautiful expression of how my approach to singing on that given Sunday was of such sensitivity that it actually made her feel heard in the listening. I have been thinking a great deal about the reflexivity of that naming by this generous human. She sensed that she had a voice, that I was honouring her listening presence, amidst the vocal expression of the song I was sharing. Let’s consider this for just a moment…the invitation into relationship that is formed through timbre and lyrical shaping. We were each caring for each other in that experience. The next morning, I participated in a virtual workshop hosted by the “Singing Side by Side” network in the UK, an interdisciplinary team of researchers with expertise in music therapy, health psychology, choir leadership and community engagement. The focus was about the musical skills that add wellbeing elements to song. And so again, the gateway to true connection in the dialogue seemed to be about the learning that comes through listening. So let’s listen, yes? Be it to your mother’s song, to your dear friend’s story, or to a graceful bird like the one soaring above me just now. Let’s commit to caring in our listening.
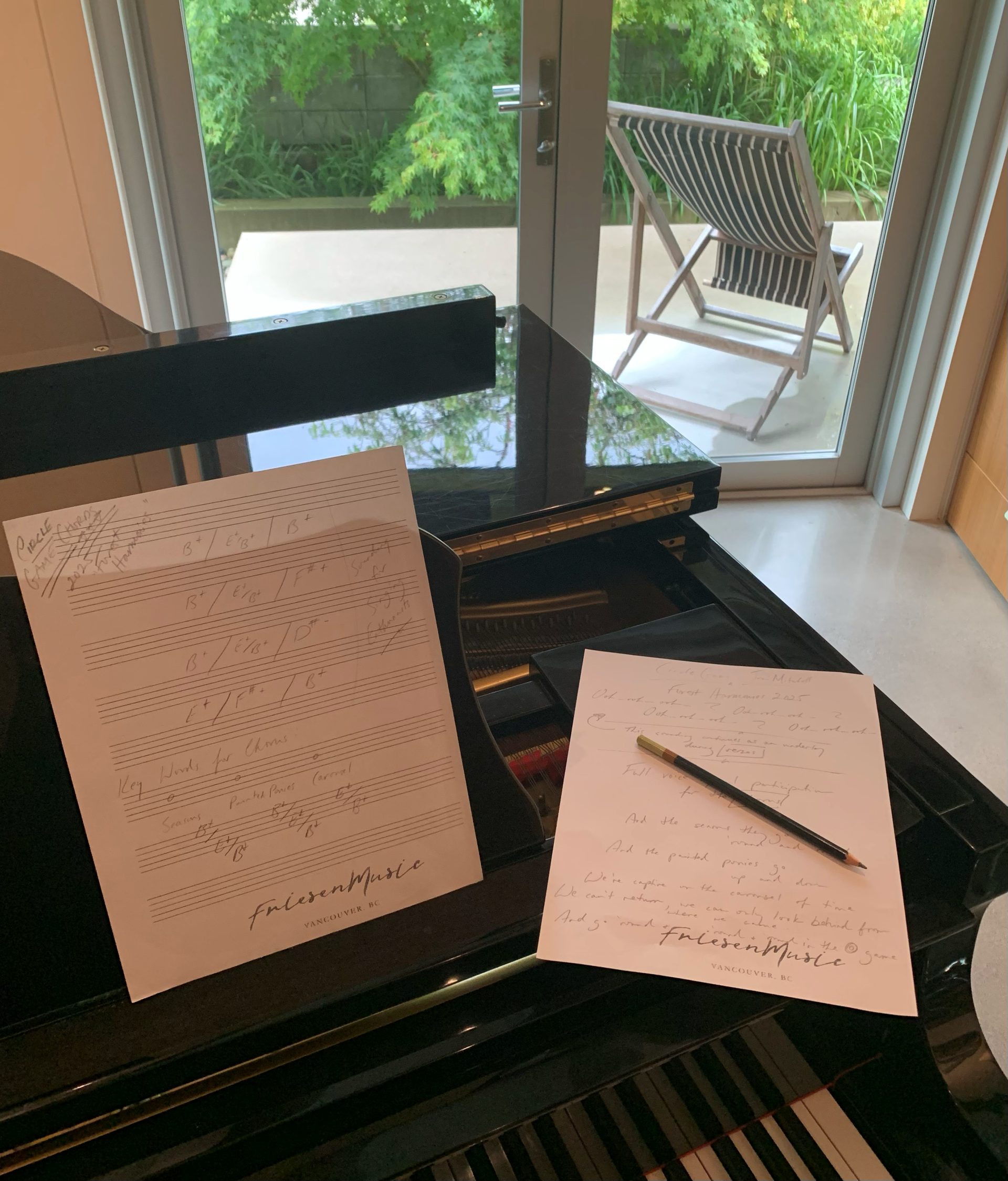
As the heat of August hints at releasin g it’s h old on us so we can step into the return of fall rhythms, I have been immersing myself in the repertoire that will potentially find expression in my classrooms and music care spaces. Some of these pieces have been at my fingertips for years, others are arrangements as new to me as they will be to those who join in the singing. We will explore melody, breath, rhythm, and phrasing together. While seeking the deeper story threads of lyrical meaning, bringing an interpretation that is uniquely ours to each composition, music’s capacity to foster relationship will undoubtedly arise yet again as a key player in our experience. It is an element of my practice that presents itself with constancy and yet, never ceases to amaze me. Perhaps you have been granted that gift of connection through song somewhere along your own distinct life path…can you transport yourself to that moment and consider its impact upon you? I recall facilitating a virtual singing session several years ago which saw me raw with emotion due to some distressing circumstances in my family circle. As much as the music educator in me was trying to maintain a certain professional veneer, I was fragile and coming undone while attempting to guide us through the songs we had hoped to sing together that day. In the final phrase of one piece, as I sought resolution in a gentle pattern of chords on the piano and exhaled deeply so as to find equilibrium, one of my participants softly asked if everything was alright . I raised my gaze, and the answer was there in my tears. The faces on my screen were just the reassurance I needed to be honest with them about my sadness. One by one, they suggested songs that they could sing for me, expressing how I didn’t even need to accompany them if I simply wanted to listen. The rest of that hour unfolded as though it were a warm embrace of care from them all. Writing about that experience now, the sense of connection is ever strong. Flowing out of this shift, reflecting on who was musically caring for whom, a realization emerged that lit a spark. We are all capable of wrapping each other up in song. A part of us is singing for our personal health and wellbeing but when we are finding our voice alongside others, we build bridges of tenderness, compassion, and empathy. I hope you’ll come along with me for this trio of reflections upon the connections which arise through song. Inhale, exhale, and be present together as we consider the ethos of musical care for one another.

