Dimensions of Music Care Part 6: Music Medicine
 In this, our sixth instalment of this blog series on the ten dimensions of music care, we are focusing on Music Medicine. The use of music for expressing emotions, or for strengthening relationships, is a familiar concept to most. Music medicine branches into new territory. With current research examining how music can be used prescriptively, the field of music medicine is emerging as an exciting, evidence-based, and generally non-invasive way to complement traditional medical interventions.
In this, our sixth instalment of this blog series on the ten dimensions of music care, we are focusing on Music Medicine. The use of music for expressing emotions, or for strengthening relationships, is a familiar concept to most. Music medicine branches into new territory. With current research examining how music can be used prescriptively, the field of music medicine is emerging as an exciting, evidence-based, and generally non-invasive way to complement traditional medical interventions.
Admittedly, music medicine is the domain of music care I often struggle to explain the most . This is likely because, like most people, my use of music is mostly based on feelings, mood, and human connection.
In my scope of practice, I use music as a relational intervention; the therapeutic impact of the music is the result of the relationship between me (the therapist), the client(s), and the music itself (ie. choices of timbre, melody, harmony, rhythm, tempo, etc.).
This relational approach is how most people engage with music for their own wellbeing. Whether we’re picking songs for a workout playlist, selecting music for a wedding ceremony, or singing to an infant, we’re focusing more on how we want the music to make us feel than we are on what its physiological impact may be.
And yet, there are always physical responses to feeling-states. The workout playlist that gets us excited will also help us run faster; the wedding music that reaches our hearts will also make us cry; the sweet lullaby we sing to our beloved baby will also put them to sleep. It is a combination of the human relationship, and the physical impact of the music, that produces these results.
In music medicine practices, these physical impacts of music are the sole focus of the interventions. While relationship between a music medicine clinician and the client may be valuable, it is not essential to the intervention’s success. The music is administered just as a prescription drug, or medical procedure – based on empirical evidence that it will create a type of physical change.
This approach may sound cold to some, as it seems to bypass that very personalized, even mystical quality of music that makes it such a cherished human language. And yet, when we start exploring the scientific evidence on music’s impact on bodies, the doors this new branch of research opens are just thrilling.
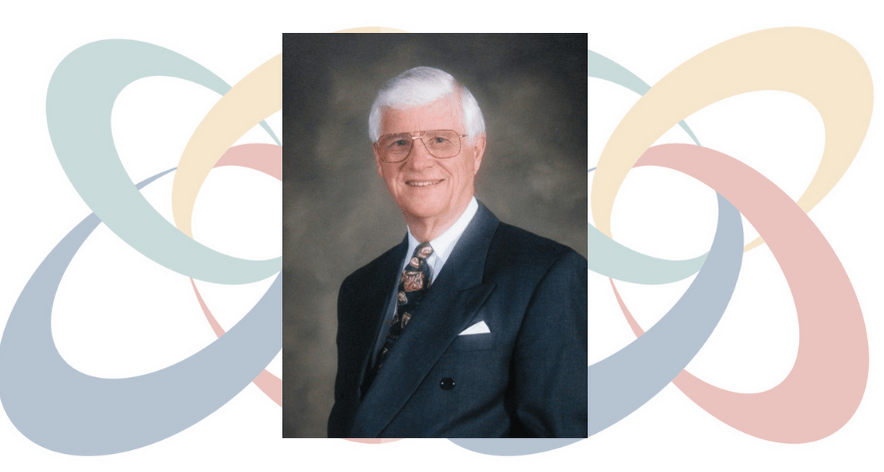
I know of no better online resource for introducing this concept than this video, linked below, featuring Dr. Lee Bartel. As he makes the distinction between music therapy and music medicine, he goes on to explain, with simple clarity, the way the brain works, the impact of brain injuries, and the unique power music can have to recover from them.
While most music medicine approaches are generally administered by skilled professionals, as with any other prescriptive practice, this research is promising for the future of medicine that incorporates this effective and non-invasive use of music for recovery.
Sarah Pearson is a music therapist working in oncology and palliative care in Kitchener, ON. She is the Program Development Lead for the Room 217 Foundation and Lead Facilitator of the Music Care Training program.