Music Education
MUSIC CARE WEBINARS
Blogs
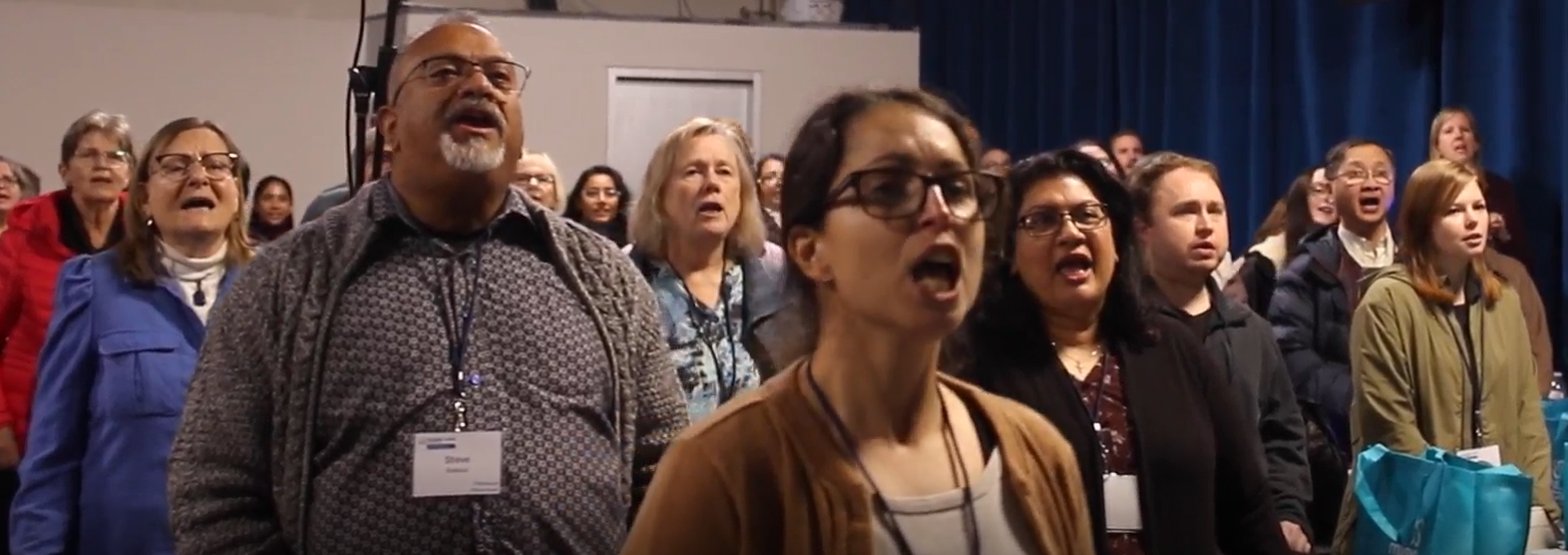
There are conferences that inform, inspire, and educate, and then there are conferences that change how we imagine what care can feel like. The Music Care Conference: The Power of a Song in Dementia Care, held at Metalworks Institute in Mississauga, was one of those rare experiences. Positioned as a national gathering that brings together people engaged in music in care across clinical, community, and educational settings, the purpose of the day became clear right from the beginning. This was not a passive event; it was an active space for co-creation and genuine connection. From the moment participants arrived, the atmosphere felt more like the start of something being built together. One of the most profound moments came during a workshop led by Bev Foster, where attendees from diverse backgrounds were to record a song together. There was no expectation of musical training or polished performance. The invitation was simply to contribute a voice and be part of the process. The piece we created was titled ‘Without a Song,’ written by Canadian singer songwriter Murray McLauchlan, and in that moment it became a shared expression of care and connection. What began as a room full of strangers gradually shifted into a connected musical space. People leaned in, listened closely, and began to sing together with growing confidence. It felt less like watching music happen and more like becoming part of something shared. In that moment, the workshop no longer felt like a breakout session. It became a living example of care expressed through music. This experience carried particular meaning in the context of dementia care. When language shifts or memory becomes harder to access, music offers a different pathway to connection, one grounded in presence. Creating music together invites participation rather than observation and can restore a sense of agency for people whose autonomy is often limited by care environments. It also strengthens relationships between caregivers and the people they support. Music does not sit on the edges of care as an added activity. It can function as care itself. The conference also highlighted that the role of music in dementia care is part of a broader shift in how the sector is evolving. With growing momentum around Bill 121, the Improving Dementia Care in Ontario Act, and increased attention from the Ministry of Long-Term Care, music is beginning to be recognized as a meaningful part of care. This commitment was reflected in a heartfelt address from Minister of Long-Term Care, Natalia Kusendova-Bashta, whose remarks affirmed the importance of dignity and compassion in dementia support. At one point she held her son at the podium and led the room in a playful rendition of ‘Baby Shark’, a moment that demonstrated how music creates connection across generations and circumstances. Policy can outline goals, but experiences like this help us imagine what care feels like when creativity and connection guide the approach. Throughout the day, research and lived practice came together through presentations from experts such as Dr. Lee Bartel, Dr. Alison Sekuler and Taylor Kurta, and through examples from organizations already integrating music-based programs in long-term care and community settings. Although the collaborative songwriting session stood out, it was one part of a day filled with meaningful experiences. The Raising Voices Dementia Choir demonstrated how music can help people living with dementia stay connected to their identity and to the people who support them. Later, the closing performance by Jill Barber brought a different dimension to the day, weaving artistry, memory, and personal storytelling into a musical experience that resonated deeply with the audience. The day also highlighted new models of community engagement such as the ‘Memories to Music’ songwriting project between the Alzheimer Society of Peel and students from Mentor College. Led by music teacher Ian Hoare and music therapist Ruth Watkiss, this initiative brings young people and persons living with dementia together to create original music, demonstrating how intergenerational collaboration can strengthen understanding and relationships across care settings. As I left the conference, I kept returning to the responsibility that comes with making music together in a care context. The song we created did not end when the session wrapped up; it became a reminder of what can happen when care is grounded in creativity and shared voice. If a group of people with no prior relationship can come together and create a shared musical experience in such a short time, then there is potential to bring this same approach into long-term care homes, community programs, hospitals, and family caregiving settings. These environments are already spaces of deep commitment and compassion, and with the right intention and support, music can help deepen relationships and strengthen the culture of care. The power of music in care is not found in adding it as a program feature; it comes from recognizing it as a way of relating to people with dignity and presence. When music becomes a shared experience, people living with dementia are included and understood rather than defined by their diagnosis. This work continues through collaborations with partners such as Acclaim Health, the Alzheimer Society of Peel, ArtsCare Mississauga, and Metalworks Institute, who help create environments where music supports meaningful connection. The music eventually came to an end, yet the song stayed with me as more than a moment from the day. It became a reminder of what can happen when care is grounded in creativity and shared voice. I left the conference with a clearer sense of how music can shape the way we support one another in real and meaningful ways. As we look ahead to the next Music Care Conference in Halifax in 2026, we carry this momentum forward, knowing that none of it happens ‘without a song’ to bring us together.

Well hello again, friends. Buoyed up by hope that my words offered here a few weeks ago have had you considering your own unique moments of being touched by music as care, I will sharpen our shared lens and share another vignette of personal experience. I have been making music in church spaces since I was very young…it is a give and take that has woven into my life rhythms as a constant beat for almost fifty years. The gratitude piece that flows through this element of musical practice is that my family of faith granted me a formative foundation from which to understand music as a spiritual gift of care. So, to recently have a woman with whom I worship Sunday after Sunday express with eloquence what it means to her to receive my playing and singing, it moved me deeply and felt worth sharing here. She is a spiritual care practitioner and a visual artist. She sees and experiences the most profound of feelings on the daily. Bonding over coffee and platz , she graced me with a beautiful expression of how my approach to singing on that given Sunday was of such sensitivity that it actually made her feel heard in the listening. I have been thinking a great deal about the reflexivity of that naming by this generous human. She sensed that she had a voice, that I was honouring her listening presence, amidst the vocal expression of the song I was sharing. Let’s consider this for just a moment…the invitation into relationship that is formed through timbre and lyrical shaping. We were each caring for each other in that experience. The next morning, I participated in a virtual workshop hosted by the “Singing Side by Side” network in the UK, an interdisciplinary team of researchers with expertise in music therapy, health psychology, choir leadership and community engagement. The focus was about the musical skills that add wellbeing elements to song. And so again, the gateway to true connection in the dialogue seemed to be about the learning that comes through listening. So let’s listen, yes? Be it to your mother’s song, to your dear friend’s story, or to a graceful bird like the one soaring above me just now. Let’s commit to caring in our listening.
Music has become for me a bit of a window into my own soul. My playlist for on the way to work enables me to be more grounded in my own beliefs and purpose as I enter into the busyness of my day to day work. Throughout the day snippets of songs come back to me and help me to refocus and also realign with my own values as I work. Sitting at the piano and playing around with melodies and lyrics opens up space in my head and my heart. Creating simple songs allows me to explore my beliefs and emotions and look deeper into my soul, finding places of peace and clarity that spill over into my interactions with family, friends, co-workers and students. Music helps me to slow down, to reflect, and to better understand myself in relation to God and the world around me. In my role as a student support teacher in an elementary school, I often use music with both adults and children. Working in a school is fast-paced with many decisions made on the fly. Teachers experience high levels of decision and compassion fatigue. They care deeply for their students and work hard to meet a wide variety of needs within their classrooms and the schools. One way I have used music is to give space and invitation for staff members to gather together and listen to music as a way to reset, reconnect and regulate during the course of a week. Listening to music has helped people to take time to process their emotions and reconnect with their purpose, giving new strength and courage to continue their important work. Working with students, I use music primarily as we look at social and emotional learning. For example, we have used an original song to help teach students internalize a process of conflict resolution that we are using to help student grow in their independent conflict management skills. Using music to help students regulate their emotions when they are upset has great benefits. This can take a number of different formats. A drumming conversation, ie. back and forth sharing of rhythms, has helped some students who are struggling to talk about what is frustrating them. The process of drumming and focusing on the rhythmic conversation frees their thinking and grows their trust enough that they are able to communicate about their big emotions. Listening to calming music can help when a student is feeling overwhelmed by their emotions. And writing songs about loss and struggle has helped some students cope with difficult situations in their lives. In my life and practice music helps build connection, community and trust allowing for deeper, more meaningful relationships that help to support students and staff learn and grow together in school.

In the first two blogs of this Key Change series, we looked at why music is considered a care solution. Undoubtedly, there is still a lot of work to do in educating the public and the care sector with a clear rationale for musical care. The bigger question, though, isn’t why music, it is how music can become integrated into the daily practice of caregivers and caring communities in a way that is meaningful, sustainable, and measurable. Many caring communities struggle to operationalize approaches like music care in a way that’s both intentional and measurable. While the research supports music’s therapeutic benefits, there’s often a disconnect between evidence and practice. The real question is how do we move from theory to everyday application? Room 217’s Integrated Model of Music Care (IMMC) is a proven framework designed to embed music into the daily practices of caregivers and care organizations. This model not only addresses cultural and contextual differences but also optimizes music in any health or social care setting. The IMMC ensures that music is not simply an add-on or an afterthought but an integral part of a care delivery system. By considering the specific needs and operational realities of an organization, this framework encourages implementation of purposeful music and sound based interventions—such as personalized playlists, music therapy, soundscapes, or community performances—tailored to improve the physical, emotional, and social well-being of everyone in the circle of care. The IMMC framework is grounded in four key components, beginning with education. Informed music use begins by training a team at the care site to champion the music care approach. With this knowledge, the team identifies a clear intention for using music to make an impact, such as reducing isolation for residents by introducing music initiatives and interventions. These can include initiatives (like a bell choir or personalized playlist) or interventions (evidence-based practices, such as those provided by a neurologic music therapist.) These initiatives are implemented through measurable programs, care tasks, or therapeutic relationships, with changes tracked through both process and outcome evaluations. Music care integration is achieved when music becomes an essential, recognized component of the care process, with all caregivers using it intentionally to address challenges in the care environment.

Health and social care leaders are tasked with making critical decisions that impact the wellbeing of both care recipients and staff. Since the COVID pandemic, we have all come to appreciate the complex challenges of providing quality care in long-term care (LTC) environments—challenges that often seem insurmountable, despite efforts to allocate resources effectively. A few years ago, I had a conversation with a newly appointed administrator in a long-term care home who asked me, "What’s so special about music?" It was a fair question. She was new to the sector, and with so many competing demands on her time and budget, she was understandably cautious about where to invest. That day, I gave her several compelling reasons why music should be a priority: it’s cost-effective, non-pharmacological, easily accessible, and most importantly, it’s part of the human experience. If I were to meet with that administrator again today, I’d focus on one key issue that’s at the heart of many care challenges: poor quality of life (QoL) for residents in long-term care, and how music care is a solution that can turn this around and quickly. Here’s why music care integration to address QoL is the investment every care leader needs to prioritize: Tangible Person-Centred Care Funding models often prioritize medical solutions over quality of life interventions, leading to institutionalized care recipients being treated as pathologies instead of people. Music, however, is an affordable, non-invasive, and customizable tool that can enrich the QoL for individuals at any stage of life. By purposefully designed music care programming, the focus can be shifted from just managing illness to fostering meaningful, person-centered care that enhances well-being. 2. Staffing and Retention The stress and burnout that care staff face is undeniable. Overworked and under-resourced teams struggle to meet the needs of care recipients, leading to high turnover and poor morale. Music care programs, which include self-care strategies for staff, create a calmer, more peaceful environment that can help reduce stress, improve job satisfaction, and bolster retention. Supporting staff resilience is essential in ensuring quality care for both residents and the workforce. Safety Safety concerns—whether physical, psychological, or environmental—are at the core of every caring community. Music care can enhance safety by reducing falls, especially during high-risk times like shift changes. Music also promotes cooperation and calm during caregiving tasks, helping care recipients feel more at ease. By incorporating mindful sound management into the environment, music helps create a safer, more comfortable space for all. Complex Care Needs Particularly in LTC, care recipients often face complex, multifaceted challenges—loneliness, pain, depression, anxiety, and behavioral issues. Music care offers a non-pharmacological, therapeutic intervention that addresses these needs without relying on medications or emergency room visits. By integrating music care into daily routines, the need for antipsychotics is reduced creating a more holistic approach to care. Operational Framework One of the biggest obstacles to music care integration is the lack of a structured framework. Without clear guidelines, standards, or expectations, music care often remains an afterthought. That’s why an evidence-based model, such as Room 217’s MUSIC CARE CERTIFY program, is critical. It promotes measurable outcomes, establishes the role of professional music care practitioners, and ensures that music care is sustainable and scalable across LTC organizations. Awareness and Advocacy While some care providers are beginning to recognize the benefits of music as a therapeutic modality, widespread public awareness and funding remain limited. Advocacy is needed by supporting music care education and public awareness campaigns. In this way, the evidence of music’s efficacy and especially for QoL, is brought to the forefront, making a compelling case for change that resonates with the LTC community and its decision-makers. Training for Healthcare Practitioners There’s currently no mandatory music care training for health and social care practitioners. While many professionals, including nurses, social workers, and recreation therapists, intuitively use music in their practice, they may not always have the tools or training to do so effectively. Providing music care skills training equips LTC staff with the confidence and knowledge to integrate music strategies responsibly and with purpose and to use it to boost their own self-care. In every meeting I have today with LTC administrators—whether they’re in suits or sweaters—I make it clear that musical care is a viable solution for ensuring good quality of life for everyone. With the right framework, education, and investment, music can be a transformative, scalable solution that impacts everyone in the circle of care.

Bono once said, "Music can change the world because it can change people." Many of us have experienced how music can shift our mood, perspective, or even deepen our sense of connection. For some, it’s a song that lifts them from a low point, for others, it might bring them closer to loved ones. In healthcare settings, music can transform not only the atmosphere but also the quality of care itself. I learned this firsthand when, during my father’s final days, my family used music to support him. We sang together to create a sense of calm, even as his medications dulled his awareness. The music allowed us to communicate and connect in a way that words alone could not. It softened the clinical nature of the hospital environment, making it a space of comfort rather than just medical procedure. Those moments had a profound impact on me, shaping my career and commitment to integrating music in healthcare spaces. For over 20 years, I’ve been dedicated to improving care through music as part of the Room 217 Foundation. We work to empower caregivers - whether paid professionals, family members or volunteers - to use music in a way that enhances the care experience. Initially, we created music tools designed to target specific care outcomes. Over time, we expanded to include training for caregivers, helping them incorporate music into everyday practice. Our latest initiative, MUSIC CARE CERTIFY (MCC), goes a step further. MCC is a comprehensive program that integrates music into the organizational culture of health and social care environments. By embedding music as a core component of care, we ensure it is sustained and becomes part of the organization’s long-term operations. One of the most powerful aspects of MCC is its focus on quality improvement. We don’t just introduce music into care settings—we measure its impact. Change isn’t just hoped for; it’s demonstrated and quantified. One standout example is the Alzheimer Society Peel (ASP), the first Canadian organization to receive MUSIC CARE Certification. This community-based organization, which serves individuals with Alzheimer’s and their families, sought to improve its acoustic environment as part of a broader commitment to enhancing care. Through a series of collaborative sound-based interventions, ASP implemented four key sound goals, evaluated through pre- and post-assessments and staff surveys. The results were compelling: Client engagement in activities increased by 75% Client wandering decreased by 40% Staff stress levels were reduced by 50% The success of this initiative underscores the tangible, measurable benefits that music can bring to care settings—improving both the experience for clients and reducing the burden on staff. In this blog series, we’ll delve deeper into Room 217’s MUSIC CARE CERTIFY as a transformative program for health and social care organizations. We’ll explore how music is not a disruptive force, but a framework for meaningful, sustainable change. With case studies from a variety of care settings across Canada, we’ll showcase how embedding music in care culture improves quality of life for all involved. Imagine a care environment where music is always accessible, integrated, and sustained! This is the future we’re working toward. Music isn’t just an art form; it’s a catalyst for measurable change in health and wellbeing. Care leaders have the power to make that change a reality within their organization. Over the next few months, our Key Change blog series will explore how the transformative power of music can improve the care experience and create lasting impact across Canada’s health and social systems. Want to learn more about MUSIC CARE CERTIFY? Come to our free, online, 45-minute Discovery session on Wednesday February 26 – 2 pm EDT. Contact Tanya for more information talbis@room217.ca

